Characteristics and Functions of Infection-enhancing Antibodies to the N-terminal Domain of SARS-CoV-2
Main Article Content
Abstract
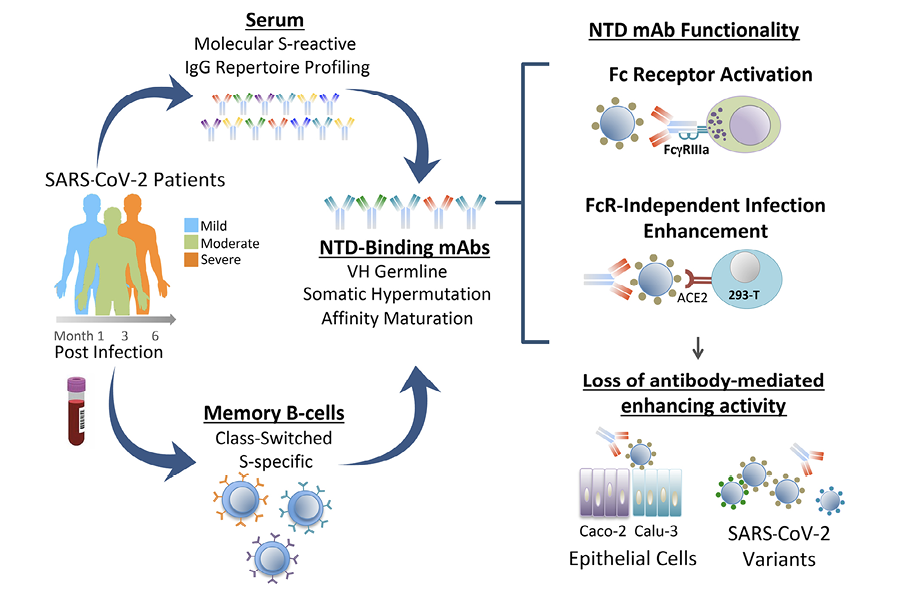
Background: Fcγ-receptor (FcγR)-independent enhancement of SARS-CoV-2 infection mediated by N-terminal domain (NTD)-binding monoclonal antibodies (mAbs) has been observed in vitro, but the functional significance of these antibodies in vivo is less clear.
Methods: We characterized 1,213 SARS-CoV-2 spike (S)-binding mAbs derived from COVID-19 convalescent patients for binding specificity to the SARS-CoV-2 S protein, VH germ-line usage, and affinity maturation. Infection enhancement in a vesicular stomatitis virus (VSV)-SARS-CoV-2 S pseudovirus (PV) assay was characterized in respiratory and intestinal epithelial cell lines, and against SARS-CoV-2 variants of concern (VOC). Proteomic deconvolution of the serum antibody repertoire was used to determine functional attributes of secreted NTD-binding mAbs.
Results: We identified 72/1213 (5.9%) mAbs that enhanced SARS-CoV-2 infection in a PV assay. The majority (68%) of these mAbs recognized the NTD, were identified in patients with mild and severe disease, and persisted for at least 5 months post-infection. Infection enhancement by NTD-binding mAbs was not observed in intestinal and respiratory epithelial cell lines and was diminished or lost against SARS-CoV-2 VOC. Proteomic deconvolution of the serum antibody repertoire from 2 of the convalescent patients identified, for the first time, NTD-binding, infection-enhancing mAbs among the circulating immunoglobulins directly isolated from serum. Functional analysis of these mAbs demonstrated robust activation of FcγRIIIa associated with antibody binding to recombinant S proteins.
Conclusions: Functionally active NTD-specific mAbs arise frequently during natural infection and can last as major serum clonotypes during convalescence. These antibodies display functional attributes that include FcγR activation, and may be selected against by mutations in NTD associated with SARS-CoV-2 VOC.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution 4.0 International License.
Pathogens and Immunity abides by Creative Commons BY 4.0:
http://creativecommons.org/licenses/by/4.0/
This license lets others distribute, remix, tweak, and build upon your work for any lawful purpose, even commercially, as long as they credit you for the original creation. This is the most accommodating of licenses offered. Recommended for maximum dissemination and use of licensed materials. The authors maintain copyright of their materal.
*Due to a template error on our pdfs, articles published from May 20, 2016 to June 24, 2022 incorrectly state the copyright is held by Pathogens and Immunity. Copyright of all articles is held by the authors of each article as noted in the above copyright policy.
References
1. Lv Z, Deng YQ, Ye Q, Cao L, Sun CY, Fan C, Huang W, Sun S, Sun Y, Zhu L, Chen Q, Wang N, Nie J, Cui Z, Zhu D, Shaw N, Li XF, Li Q, Xie L, Wang Y, Rao Z, Qin CF, Wang X. Structural basis for neutralization of SARS-CoV-2 and SARS-CoV by a potent therapeutic antibody. Science. 2020;369(6510):1505-9. doi: 10.1126/science.abc5881. PubMed PMID: 32703908; PMCID: PMC7402622.
DOI: https://doi.org/10.1126/science.abc58812. Salazar E, Kuchipudi SV, Christensen PA, Eagar T, Yi X, Zhao P, Jin Z, Long SW, Olsen RJ, Chen J, Castillo B, Leveque C, Towers D, Lavinder J, Gollihar J, Cardona J, Ippolito G, Nissly R, Bird I, Greenawalt D, Rossi RM, Gontu A, Srinivasan S, Poojary I, Cattadori IM, Hudson PJ, Josleyn NM, Prugar L, Huie K, Herbert A, Bernard DW, Dye JM, Kapur V, Musser JM. Convalescent plasma anti-SARS-CoV-2 spike protein ectodomain and receptor-binding domain IgG correlate with virus neutralization. J Clin Invest. 2020;130(12):6728-38. doi: 10.1172/JCI141206. PubMed PMID: 32910806; PMCID: PMC7685744.
DOI: https://doi.org/10.1172/JCI1412063. Stamatatos L, Czartoski J, Wan YH, Homad LJ, Rubin V, Glantz H, Neradilek M, Seydoux E, Jennewein MF, MacCamy AJ, Feng J, Mize G, De Rosa SC, Finzi A, Lemos MP, Cohen KW, Moodie Z, McElrath MJ, McGuire AT. mRNA vaccination boosts cross-variant neutralizing antibodies elicited by SARS-CoV-2 infection. Science. 2021;372(6549):1413-8. doi: 10.1126/science.abg9175. PubMed PMID: 33766944; PMCID: PMC8139425.
DOI: https://doi.org/10.1126/science.abg91754. Wec AZ, Wrapp D, Herbert AS, Maurer DP, Haslwanter D, Sakharkar M, Jangra RK, Dieterle ME, Lilov A, Huang D, Tse LV, Johnson NV, Hsieh CL, Wang N, Nett JH, Champney E, Burnina I, Brown M, Lin S, Sinclair M, Johnson C, Pudi S, Bortz R, 3rd, Wirchnianski AS, Laudermilch E, Florez C, Fels JM, O’Brien CM, Graham BS, Nemazee D, Burton DR, Baric RS, Voss JE, Chandran K, Dye JM, McLellan JS, Walker LM. Broad neutralization of SARS-related viruses by human monoclonal antibodies. Science. 2020;369(6504):731-6. doi: 10.1126/science.abc7424. PubMed PMID: 32540900; PMCID: PMC7299279.
DOI: https://doi.org/10.1126/science.abc74245. Chen RE, Zhang X, Case JB, Winkler ES, Liu Y, VanBlargan LA, Liu J, Errico JM, Xie X, Suryadevara N, Gilchuk P, Zost SJ, Tahan S, Droit L, Turner JS, Kim W, Schmitz AJ, Thapa M, Wang D, Boon ACM, Presti RM, O’Halloran JA, Kim AHJ, Deepak P, Pinto D, Fremont DH, Crowe JE, Jr., Corti D, Virgin HW, Ellebedy AH, Shi PY, Diamond MS. Resistance of SARS-CoV-2 variants to neutralization by monoclonal and serum-derived polyclonal antibodies. Nat Med. 2021;27(4):717-26. doi: 10.1038/s41591-021-01294-w. PubMed PMID: 33664494; PMCID: PMC8058618.
DOI: https://doi.org/10.1038/s41591-021-01294-w6. Garcia-Beltran WF, Lam EC, St Denis K, Nitido AD, Garcia ZH, Hauser BM, Feldman J, Pavlovic MN, Gregory DJ, Poznansky MC, Sigal A, Schmidt AG, Iafrate AJ, Naranbhai V, Balazs AB. Multiple SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity. Cell. 2021;184(9):2372-83 e9. doi: 10.1016/j.cell.2021.03.013. PubMed PMID: 33743213; PMCID: PMC7953441.
DOI: https://doi.org/10.1016/j.cell.2021.03.0137. Liu Z, VanBlargan LA, Bloyet LM, Rothlauf PW, Chen RE, Stumpf S, Zhao H, Errico JM, Theel ES, Liebeskind MJ, Alford B, Buchser WJ, Ellebedy AH, Fremont DH, Diamond MS, Whelan SPJ. Identification of SARS-CoV-2 spike mutations that attenuate monoclonal and serum antibody neutralization. Cell Host Microbe. 2021;29(3):477-88 e4. doi: 10.1016/j.chom.2021.01.014. PubMed PMID: 33535027; PMCID: PMC7839837.
DOI: https://doi.org/10.1016/j.chom.2021.01.0148. Harvey WT, Carabelli AM, Jackson B, Gupta RK, Thomson EC, Harrison EM, Ludden C, Reeve R, Rambaut A, Consortium C-GU, Peacock SJ, Robertson DL. SARS-CoV-2 variants, spike mutations and immune escape. Nat Rev Microbiol. 2021;19(7):409-24. doi: 10.1038/s41579-021-00573-0. PubMed PMID: 34075212; PMCID: PMC8167834.
DOI: https://doi.org/10.1038/s41579-021-00573-09. Cantoni D, Murray MJ, Kalemera MD, Dicken SJ, Stejskal L, Brown G, Lytras S, Coey JD, McKenna J, Bridgett S, Simpson D, Fairley D, Thorne LG, Reuschl AK, Forrest C, Ganeshalingham M, Muir L, Palor M, Jarvis L, Willett B, Power UF, McCoy LE, Jolly C, Towers GJ, Doores KJ, Robertson DL, Shepherd AJ, Reeves MB, Bamford CGG, Grove J. Evolutionary remodelling of N-terminal domain loops fine-tunes SARS-CoV-2 spike. EMBO Rep. 2022;23(10):e54322. doi: 10.15252/embr.202154322. PubMed PMID: 35999696; PMCID: PMC9535765.
DOI: https://doi.org/10.15252/embr.20215432210. Gong Y, Qin S, Dai L, Tian Z. The glycosylation in SARS-CoV-2 and its receptor ACE2. Signal Transduct Target Ther. 2021;6(1):396. doi: 10.1038/s41392-021-00809-8. PubMed PMID: 34782609; PMCID: PMC8591162.
DOI: https://doi.org/10.1038/s41392-021-00809-811. Seyran M, Takayama K, Uversky VN, Lundstrom K, Palu G, Sherchan SP, Attrish D, Rezaei N, Aljabali AAA, Ghosh S, Pizzol D, Chauhan G, Adadi P, Mohamed Abd El-Aziz T, Soares AG, Kandimalla R, Tambuwala M, Hassan SS, Azad GK, Pal Choudhury P, Baetas-da-Cruz W, Serrano-Aroca A, Brufsky AM, Uhal BD. The structural basis of accelerated host cell entry by SARS-CoV-2dagger. FEBS J. 2021;288(17):5010-20. doi: 10.1111/febs.15651. PubMed PMID: 33264497; PMCID: PMC7753708.
DOI: https://doi.org/10.1111/febs.1565112. Soh WTL, Y.; Nakayama, E. E.; Ono, C.; Torii, S.; Nakagami, H.; Matsuura,Y.; Shioda, T.; Arase, H. The N-terminal domain of spike glycoprotein mediates SARS-CoV-2 infection by associating with L-SIGN and DC-SIGN. bioRxiv. 2020. doi: 10.1101/2020.11.05.369264.
13. Cerutti G, Guo Y, Zhou T, Gorman J, Lee M, Rapp M, Reddem ER, Yu J, Bahna F, Bimela J, Huang Y, Katsamba PS, Liu L, Nair MS, Rawi R, Olia AS, Wang P, Zhang B, Chuang GY, Ho DD, Sheng Z, Kwong PD, Shapiro L. Potent SARS-CoV-2 neutralizing antibodies directed against spike N-terminal domain target a single supersite. Cell Host Microbe. 2021;29(5):819-33 e7. doi: 10.1016/j.chom.2021.03.005. PubMed PMID: 33789084; PMCID: PMC7953435.
DOI: https://doi.org/10.1016/j.chom.2021.03.00514. Chi X, Yan R, Zhang J, Zhang G, Zhang Y, Hao M, Zhang Z, Fan P, Dong Y, Yang Y, Chen Z, Guo Y, Zhang J, Li Y, Song X, Chen Y, Xia L, Fu L, Hou L, Xu J, Yu C, Li J, Zhou Q, Chen W. A neutralizing human antibody binds to the N-terminal domain of the Spike protein of SARS-CoV-2. Science. 2020;369(6504):650-5. doi: 10.1126/science.abc6952. PubMed PMID: 32571838; PMCID: PMC7319273.
DOI: https://doi.org/10.1126/science.abc695215. McCallum M, De Marco A, Lempp FA, Tortorici MA, Pinto D, Walls AC, Beltramello M, Chen A, Liu Z, Zatta F, Zepeda S, di Iulio J, Bowen JE, Montiel-Ruiz M, Zhou J, Rosen LE, Bianchi S, Guarino B, Fregni CS, Abdelnabi R, Foo SC, Rothlauf PW, Bloyet LM, Benigni F, Cameroni E, Neyts J, Riva A, Snell G, Telenti A, Whelan SPJ, Virgin HW, Corti D, Pizzuto MS, Veesler D. N-terminal domain antigenic mapping reveals a site of vulnerability for SARS-CoV-2. Cell. 2021;184(9):2332-47 e16. doi: 10.1016/j.cell.2021.03.028. PubMed PMID: 33761326; PMCID: PMC7962585.
DOI: https://doi.org/10.1016/j.cell.2021.03.02816. Suryadevara N, Shrihari S, Gilchuk P, VanBlargan LA, Binshtein E, Zost SJ, Nargi RS, Sutton RE, Winkler ES, Chen EC, Fouch ME, Davidson E, Doranz BJ, Chen RE, Shi PY, Carnahan RH, Thackray LB, Diamond MS, Crowe JE, Jr. Neutralizing and protective human monoclonal antibodies recognizing the N-terminal domain of the SARS-CoV-2 spike protein. Cell. 2021;184(9):2316-31 e15. doi: 10.1016/j.cell.2021.03.029. PubMed PMID: 33773105; PMCID: PMC7962591.
DOI: https://doi.org/10.1016/j.cell.2021.03.02917. Voss WN, Hou YJ, Johnson NV, Delidakis G, Kim JE, Javanmardi K, Horton AP, Bartzoka F, Paresi CJ, Tanno Y, Chou CW, Abbasi SA, Pickens W, George K, Boutz DR, Towers DM, McDaniel JR, Billick D, Goike J, Rowe L, Batra D, Pohl J, Lee J, Gangappa S, Sambhara S, Gadush M, Wang N, Person MD, Iverson BL, Gollihar JD, Dye JM, Herbert AS, Finkelstein IJ, Baric RS, McLellan JS, Georgiou G, Lavinder JJ, Ippolito GC. Prevalent, protective, and convergent IgG recognition of SARS-CoV-2 non-RBD spike epitopes. Science. 2021;372(6546):1108-12. doi: 10.1126/science.abg5268. PubMed PMID: 33947773; PMCID: PMC8224265.
DOI: https://doi.org/10.1126/science.abg526818. Wang Z, Muecksch F, Cho A, Gaebler C, Hoffmann HH, Ramos V, Zong S, Cipolla M, Johnson B, Schmidt F, DaSilva J, Bednarski E, Ben Tanfous T, Raspe R, Yao K, Lee YE, Chen T, Turroja M, Milard KG, Dizon J, Kaczynska A, Gazumyan A, Oliveira TY, Rice CM, Caskey M, Bieniasz PD, Hatziioannou T, Barnes CO, Nussenzweig MC. Analysis of memory B cells identifies conserved neutralizing epitopes on the N-terminal domain of variant SARS-Cov-2 spike proteins. Immunity. 2022;55(6):998-1012 e8. doi: 10.1016/j.immuni.2022.04.003. PubMed PMID: 35447092; PMCID: PMC8986478.
DOI: https://doi.org/10.1016/j.immuni.2022.04.00319. Li D, Edwards RJ, Manne K, Martinez DR, Schafer A, Alam SM, Wiehe K, Lu X, Parks R, Sutherland LL, Oguin TH, 3rd, McDanal C, Perez LG, Mansouri K, Gobeil SMC, Janowska K, Stalls V, Kopp M, Cai F, Lee E, Foulger A, Hernandez GE, Sanzone A, Tilahun K, Jiang C, Tse LV, Bock KW, Minai M, Nagata BM, Cronin K, Gee-Lai V, Deyton M, Barr M, Von Holle T, Macintyre AN, Stover E, Feldman J, Hauser BM, Caradonna TM, Scobey TD, Rountree W, Wang Y, Moody MA, Cain DW, DeMarco CT, Denny TN, Woods CW, Petzold EW, Schmidt AG, Teng IT, Zhou T, Kwong PD, Mascola JR, Graham BS, Moore IN, Seder R, Andersen H, Lewis MG, Montefiori DC, Sempowski GD, Baric RS, Acharya P, Haynes BF, Saunders KO. In vitro and in vivo functions of SARS-CoV-2 infection-enhancing and neutralizing antibodies. Cell. 2021;184(16):4203-19 e32. doi: 10.1016/j.cell.2021.06.021. PubMed PMID: 34242577; PMCID: PMC8232969.
DOI: https://doi.org/10.1016/j.cell.2021.06.02120. Liu Y, Soh WT, Kishikawa JI, Hirose M, Nakayama EE, Li S, Sasai M, Suzuki T, Tada A, Arakawa A, Matsuoka S, Akamatsu K, Matsuda M, Ono C, Torii S, Kishida K, Jin H, Nakai W, Arase N, Nakagawa A, Matsumoto M, Nakazaki Y, Shindo Y, Kohyama M, Tomii K, Ohmura K, Ohshima S, Okamoto T, Yamamoto M, Nakagami H, Matsuura Y, Nakagawa A, Kato T, Okada M, Standley DM, Shioda T, Arase H. An infectivity-enhancing site on the SARS-CoV-2 spike protein targeted by antibodies. Cell. 2021;184(13):3452-66 e18. doi: 10.1016/j.cell.2021.05.032. PubMed PMID: 34139176; PMCID: PMC8142859.
DOI: https://doi.org/10.1016/j.cell.2021.05.03221. Beaudoin-Bussieres G, Chen Y, Ullah I, Prevost J, Tolbert WD, Symmes K, Ding S, Benlarbi M, Gong SY, Tauzin A, Gasser R, Chatterjee D, Vezina D, Goyette G, Richard J, Zhou F, Stamatatos L, McGuire AT, Charest H, Roger M, Pozharski E, Kumar P, Mothes W, Uchil PD, Pazgier M, Finzi A. A Fc-enhanced NTD-binding non-neutralizing antibody delays virus spread and synergizes with a nAb to protect mice from lethal SARS-CoV-2 infection. Cell Rep. 2022;38(7):110368. doi: 10.1016/j.celrep.2022.110368. PubMed PMID: 35123652; PMCID: PMC8786652.
DOI: https://doi.org/10.1016/j.celrep.2022.11036822. Sakharkar M, Rappazzo CG, Wieland-Alter WF, Hsieh CL, Wrapp D, Esterman ES, Kaku CI, Wec AZ, Geoghegan JC, McLellan JS, Connor RI, Wright PF, Walker LM. Prolonged evolution of the human B cell response to SARS-CoV-2 infection. Sci Immunol. 2021;6(56). doi: 10.1126/sciimmunol.abg6916. PubMed PMID: 33622975; PMCID: PMC8128290.
DOI: https://doi.org/10.1126/sciimmunol.abg691623. Wright PF, Prevost-Reilly AC, Natarajan H, Brickley EB, Connor RI, Wieland-Alter WF, Miele AS, Weiner JA, Nerenz RD, Ackerman ME. Longitudinal Systemic and Mucosal Immune Responses to SARS-CoV-2 Infection. J Infect Dis. 2022;226(7):1204-14. doi: 10.1093/infdis/jiac065. PubMed PMID: 35188974; PMCID: PMC8903457.
DOI: https://doi.org/10.1093/infdis/jiac06524. Butler SE, Crowley AR, Natarajan H, Xu S, Weiner JA, Bobak CA, Mattox DE, Lee J, Wieland-Alter W, Connor RI, Wright PF, Ackerman ME. Distinct Features and Functions of Systemic and Mucosal Humoral Immunity Among SARS-CoV-2 Convalescent Individuals. Front Immunol. 2020;11:618685. doi: 10.3389/fimmu.2020.618685. PubMed PMID: 33584712; PMCID: PMC7876222.
DOI: https://doi.org/10.3389/fimmu.2020.61868525. Natarajan H, Crowley AR, Butler SE, Xu S, Weiner JA, Bloch EM, Littlefield K, Wieland-Alter W, Connor RI, Wright PF, Benner SE, Bonny TS, Laeyendecker O, Sullivan D, Shoham S, Quinn TC, Larman HB, Casadevall A, Pekosz A, Redd AD, Tobian AAR, Ackerman ME. Markers of Polyfunctional SARS-CoV-2 Antibodies in Convalescent Plasma. mBio. 2021;12(2). doi: 10.1128/mBio.00765-21. PubMed PMID: 33879585; PMCID: PMC8092262.
DOI: https://doi.org/10.1128/mBio.00765-2126. Curtis NC, Shin S, Hederman AP, Connor RI, Wieland-Alter WF, Ionov S, Boylston J, Rose J, Sakharkar M, Dorman DB, Dessaint JA, Gwilt LL, Crowley AR, Feldman J, Hauser BM, Schmidt AG, Ashare A, Walker LM, Wright PF, Ackerman ME, Lee J. Characterization of SARS-CoV-2 Convalescent Patients’ Serological Repertoire Reveals High Prevalence of Iso-RBD Antibodies. bioRxiv. 2023. doi: 10.1101/2023.09.08.556349. PubMed PMID: 37745524; PMCID: PMC10515772.
DOI: https://doi.org/10.1101/2023.09.08.55634927. Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5(4):562-9. doi: 10.1038/s41564-020-0688-y. PubMed PMID: 32094589; PMCID: PMC7095430.
DOI: https://doi.org/10.1038/s41564-020-0688-y28. Cho H, Gonzales-Wartz KK, Huang D, Yuan M, Peterson M, Liang J, Beutler N, Torres JL, Cong Y, Postnikova E, Bangaru S, Talana CA, Shi W, Yang ES, Zhang Y, Leung K, Wang L, Peng L, Skinner J, Li S, Wu NC, Liu H, Dacon C, Moyer T, Cohen M, Zhao M, Lee FE, Weinberg RS, Douagi I, Gross R, Schmaljohn C, Pegu A, Mascola JR, Holbrook M, Nemazee D, Rogers TF, Ward AB, Wilson IA, Crompton PD, Tan J. Bispecific antibodies targeting distinct regions of the spike protein potently neutralize SARS-CoV-2 variants of concern. Sci Transl Med. 2021;13(616):eabj5413. doi: 10.1126/scitranslmed.abj5413. PubMed PMID: 34519517; PMCID: PMC8651051.
DOI: https://doi.org/10.1126/scitranslmed.abj541329. Garcia-Beltran WF, St Denis KJ, Hoelzemer A, Lam EC, Nitido AD, Sheehan ML, Berrios C, Ofoman O, Chang CC, Hauser BM, Feldman J, Roederer AL, Gregory DJ, Poznansky MC, Schmidt AG, Iafrate AJ, Naranbhai V, Balazs AB. mRNA-based COVID-19 vaccine boosters induce neutralizing immunity against SARS-CoV-2 Omicron variant. Cell. 2022;185(3):457-66 e4. doi: 10.1016/j.cell.2021.12.033. PubMed PMID: 34995482; PMCID: PMC8733787.
DOI: https://doi.org/10.1016/j.cell.2021.12.03330. Dacon C, Tucker C, Peng L, Lee CD, Lin TH, Yuan M, Cong Y, Wang L, Purser L, Williams JK, Pyo CW, Kosik I, Hu Z, Zhao M, Mohan D, Cooper AJR, Peterson M, Skinner J, Dixit S, Kollins E, Huzella L, Perry D, Byrum R, Lembirik S, Drawbaugh D, Eaton B, Zhang Y, Yang ES, Chen M, Leung K, Weinberg RS, Pegu A, Geraghty DE, Davidson E, Douagi I, Moir S, Yewdell JW, Schmaljohn C, Crompton PD, Holbrook MR, Nemazee D, Mascola JR, Wilson IA, Tan J. Broadly neutralizing antibodies target the coronavirus fusion peptide. Science. 2022;377(6607):728-35. doi: 10.1126/science.abq3773. PubMed PMID: 35857439; PMCID: PMC9348754.
DOI: https://doi.org/10.1126/science.abq377331. Yahi N, Chahinian H, Fantini J. Infection-enhancing anti-SARS-CoV-2 antibodies recognize both the original Wuhan/D614G strain and Delta variants. A potential risk for mass vaccination? J Infect. 2021;83(5):607-35. doi: 10.1016/j.jinf.2021.08.010. PubMed PMID: 34384810; PMCID: PMC8351274.
DOI: https://doi.org/10.1016/j.jinf.2021.08.01032. Aguiar JA, Tremblay BJ, Mansfield MJ, Woody O, Lobb B, Banerjee A, Chandiramohan A, Tiessen N, Cao Q, Dvorkin-Gheva A, Revill S, Miller MS, Carlsten C, Organ L, Joseph C, John A, Hanson P, Austin RC, McManus BM, Jenkins G, Mossman K, Ask K, Doxey AC, Hirota JA. Gene expression and in situ protein profiling of candidate SARS-CoV-2 receptors in human airway epithelial cells and lung tissue. Eur Respir J. 2020;56(3). doi: 10.1183/13993003.01123-2020. PubMed PMID: 32675206; PMCID: PMC7366180.
DOI: https://doi.org/10.1183/13993003.01123-202033. Hou YJ, Okuda K, Edwards CE, Martinez DR, Asakura T, Dinnon KH, 3rd, Kato T, Lee RE, Yount BL, Mascenik TM, Chen G, Olivier KN, Ghio A, Tse LV, Leist SR, Gralinski LE, Schafer A, Dang H, Gilmore R, Nakano S, Sun L, Fulcher ML, Livraghi-Butrico A, Nicely NI, Cameron M, Cameron C, Kelvin DJ, de Silva A, Margolis DM, Markmann A, Bartelt L, Zumwalt R, Martinez FJ, Salvatore SP, Borczuk A, Tata PR, Sontake V, Kimple A, Jaspers I, O’Neal WK, Randell SH, Boucher RC, Baric RS. SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract. Cell. 2020;182(2):429-46 e14. doi: 10.1016/j.cell.2020.05.042. PubMed PMID: 32526206; PMCID: PMC7250779.
DOI: https://doi.org/10.1016/j.cell.2020.05.04234. Li MY, Li L, Zhang Y, Wang XS. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty. 2020;9(1):45. doi: 10.1186/s40249-020-00662-x. PubMed PMID: 32345362; PMCID: PMC7186534.
DOI: https://doi.org/10.1186/s40249-020-00662-x35. Wang Y, Wang Y, Luo W, Huang L, Xiao J, Li F, Qin S, Song X, Wu Y, Zeng Q, Jin F, Wang Y. A comprehensive investigation of the mRNA and protein level of ACE2, the putative receptor of SARS-CoV-2, in human tissues and blood cells. Int J Med Sci. 2020;17(11):1522-31. doi: 10.7150/ijms.46695. PubMed PMID: 32669955; PMCID: PMC7359402.
DOI: https://doi.org/10.7150/ijms.4669536. ter Meulen J, van den Brink EN, Poon LL, Marissen WE, Leung CS, Cox F, Cheung CY, Bakker AQ, Bogaards JA, van Deventer E, Preiser W, Doerr HW, Chow VT, de Kruif J, Peiris JS, Goudsmit J. Human monoclonal antibody combination against SARS coronavirus: synergy and coverage of escape mutants. PLoS Med. 2006;3(7):e237. doi: 10.1371/journal.pmed.0030237. PubMed PMID: 16796401; PMCID: PMC1483912.
DOI: https://doi.org/10.1371/journal.pmed.003023737. Wang Z, Muecksch F, Schaefer-Babajew D, Finkin S, Viant C, Gaebler C, Hoffmann HH, Barnes CO, Cipolla M, Ramos V, Oliveira TY, Cho A, Schmidt F, Da Silva J, Bednarski E, Aguado L, Yee J, Daga M, Turroja M, Millard KG, Jankovic M, Gazumyan A, Zhao Z, Rice CM, Bieniasz PD, Caskey M, Hatziioannou T, Nussenzweig MC. Naturally enhanced neutralizing breadth against SARS-CoV-2 one year after infection. Nature. 2021;595(7867):426-31. doi: 10.1038/s41586-021-03696-9. PubMed PMID: 34126625; PMCID: PMC8277577.
DOI: https://doi.org/10.1038/s41586-021-03696-938. Yuan M, Wu NC, Zhu X, Lee CD, So RTY, Lv H, Mok CKP, Wilson IA. A highly conserved cryptic epitope in the receptor binding domains of SARS-CoV-2 and SARS-CoV. Science. 2020;368(6491):630-3. doi: 10.1126/science.abb7269. PubMed PMID: 32245784; PMCID: PMC7164391.
DOI: https://doi.org/10.1126/science.abb726939. Chu H, Chan JF, Yuen TT, Shuai H, Yuan S, Wang Y, Hu B, Yip CC, Tsang JO, Huang X, Chai Y, Yang D, Hou Y, Chik KK, Zhang X, Fung AY, Tsoi HW, Cai JP, Chan WM, Ip JD, Chu AW, Zhou J, Lung DC, Kok KH, To KK, Tsang OT, Chan KH, Yuen KY. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. Lancet Microbe. 2020;1(1):e14-e23. doi: 10.1016/S2666-5247(20)30004-5. PubMed PMID: 32835326; PMCID: PMC7173822.
DOI: https://doi.org/10.1016/S2666-5247(20)30004-540. Feng XL, Yu D, Zhang M, Li X, Zou QC, Ma W, Han JB, Xu L, Yang C, Qu W, Deng ZH, Long J, Long Y, Li M, Yao YG, Dong XQ, Zeng J, Li MH. Characteristics of replication and pathogenicity of SARS-CoV-2 Alpha and Delta isolates. Virol Sin. 2022;37(6):804-12. doi: 10.1016/j.virs.2022.09.007. PubMed PMID: 36167254; PMCID: PMC9507998.
DOI: https://doi.org/10.1016/j.virs.2022.09.00741. Jureka AS, Basler CF. Propagation and Quantification of SARS-CoV-2. Methods Mol Biol. 2022;2452:111-29. doi: 10.1007/978-1-0716-2111-0_8. PubMed PMID: 35554904.
42. Mautner L, Hoyos M, Dangel A, Berger C, Ehrhardt A, Baiker A. Replication kinetics and infectivity of SARS-CoV-2 variants of concern in common cell culture models. Virol J. 2022;19(1):76. doi: 10.1186/s12985-022-01802-5. PubMed PMID: 35473640; PMCID: PMC9038516.
DOI: https://doi.org/10.1186/s12985-022-01802-543. Rajah MM, Hubert M, Bishop E, Saunders N, Robinot R, Grzelak L, Planas D, Dufloo J, Gellenoncourt S, Bongers A, Zivaljic M, Planchais C, Guivel-Benhassine F, Porrot F, Mouquet H, Chakrabarti LA, Buchrieser J, Schwartz O. SARS-CoV-2 Alpha, Beta, and Delta variants display enhanced Spike-mediated syncytia formation. EMBO J. 2021;40(24):e108944. doi: 10.15252/embj.2021108944. PubMed PMID: 34601723; PMCID: PMC8646911.
DOI: https://doi.org/10.15252/embj.202110894444. Ren X, Glende J, Al-Falah M, de Vries V, Schwegmann-Wessels C, Qu X, Tan L, Tschernig T, Deng H, Naim HY, Herrler G. Analysis of ACE2 in polarized epithelial cells: surface expression and function as receptor for severe acute respiratory syndrome-associated coronavirus. J Gen Virol. 2006;87(Pt 6):1691-5. doi: 10.1099/vir.0.81749-0. PubMed PMID: 16690935.
DOI: https://doi.org/10.1099/vir.0.81749-045. Farrell AG, Dadonaite B, Greaney AJ, Eguia R, Loes AN, Franko NM, Logue J, Carreno JM, Abbad A, Chu HY, Matreyek KA, Bloom JD. Receptor-Binding Domain (RBD) Antibodies Contribute More to SARS-CoV-2 Neutralization When Target Cells Express High Levels of ACE2. Viruses. 2022;14(9). doi: 10.3390/v14092061. PubMed PMID: 36146867; PMCID: PMC9504593.
DOI: https://doi.org/10.3390/v1409206146. Gerdol M, Dishnica K, Giorgetti A. Emergence of a recurrent insertion in the N-terminal domain of the SARS-CoV-2 spike glycoprotein. Virus Res. 2022;310:198674. doi: 10.1016/j.virusres.2022.198674. PubMed PMID: 35021068; PMCID: PMC8743576.
DOI: https://doi.org/10.1016/j.virusres.2022.19867447. Pettersen EF, Goddard TD, Huang CC, Couch GS, Greenblatt DM, Meng EC, Ferrin TE. UCSF Chimera--a visualization system for exploratory research and analysis. J Comput Chem. 2004;25(13):1605-12. doi: 10.1002/jcc.20084. PubMed PMID: 15264254.
DOI: https://doi.org/10.1002/jcc.2008448. Sali A. Comparative protein modeling by satisfaction of spatial restraints. Mol Med Today. 1995;1(6):270-7. doi: 10.1016/s1357-4310(95)91170-7. PubMed PMID: 9415161.
DOI: https://doi.org/10.1016/S1357-4310(95)91170-7